NuDESC Screening Alert
This patient has screened positive for delirium.
(i.e., their Nursing Delirium Screening Scale [NuDESC] score is 2 or greater.)
What is Delirium?
Delirium is an acute state of confusion that results in acute or fluctuating decline in attention and cognition.
Delirium is usually evidence of an underlying physiologic or medical problem.
Why Does Delirium Matter?
Delirium is common: 25-75% prevalence in the hospital.
Delirium is commonly missed - in up to 70% of cases.
Delirium is associated with poor outcomes (even after adjusting for age, comorbid illness, or a diagnosis of dementia), including:
- Functional and cognitive decline (acute and long-term)
- Longer hospital stays
- Higher risk for institutionalization (read: nursing home placement)
- Higher risk for mortality (up to 2x-4x mortality at 6-12 months)
For these reasons, delirium is considered an important healthcare quality indicator for older adults.
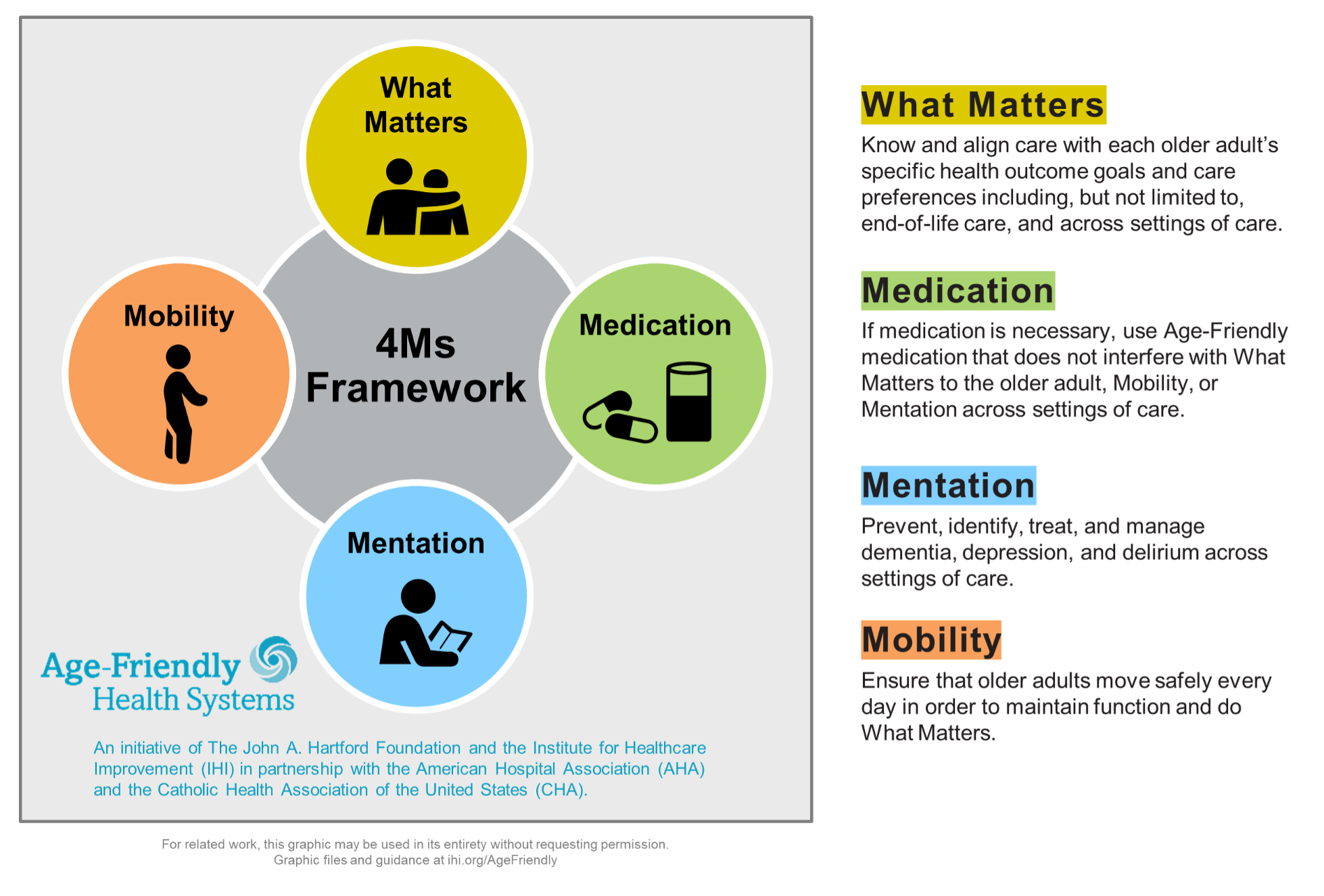
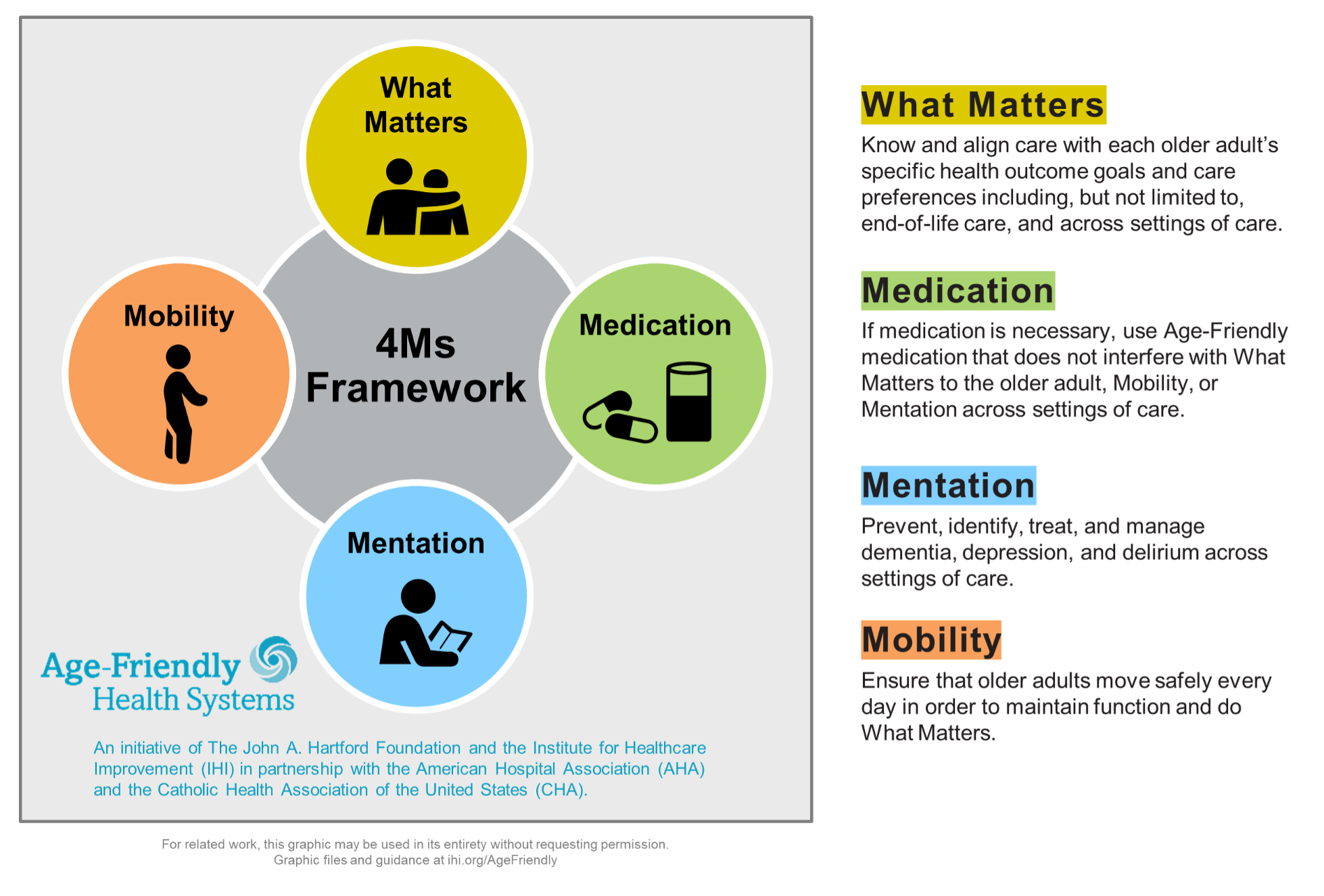
4 Ms Of Age-Friendly Care
Delirium is a key element of the “Mentation” M of the 4 Ms of Age-Friendly Care.
Delirium Quick List
Actions to Consider:
- Consider hyperacute causes (MI, PE, stroke/ICH, seizure, sepsis)
- Consider drug intoxication or withdrawal
- Consider HIGH RISK medications* as below, which may cause or worsen delirium
- MINIMIZE new Rx’s for such medications in patients who are NuDESC(+)
Non-pharmacologic measures to improve delirium and prevent further episodes:
- Provide sensory/functional aids: hearing aids, eyeglasses, dentures
- Promote normal sleep/wake: lights on during daytime; minimize nighttime interruptions
- Encourage family involvement; ask them to bring activities the patient enjoys
- Minimize unnecessary tethers (telemetry, restraints, foley catheters, etc.)
- Reorient the patient frequently to time, place, and situation
- Minimize NPO time as able; optimize nutrition; treat dehydration
- Treat pain promptly
- Treat constipation and urinary retention
- Optimize mobility: set challenging mobility goals each day and follow up on those goals
- Ensure home CPAP/BiPAP is ordered/use, if applicable
- Consider consultation with geriatrics (for 65+), behavioral health, and/or neurology as appropriate
HIGH RISK MEDICATIONS IN DELIRIUM INCLUDE:
- Anticholinergics (e.g., scopolamine)
- Antihistamines (e.g., diphenhydramine)
- Benzodiazepines (e.g., lorazepam)
- Corticosteroids
- Opioids
- Antispasmodics (e.g., cyclobenzaprine)
Note: These medications can directly cause or worsen delirium, especially in frail older adults.
Many patients require tapering of the above medications rather than abrupt discontinuation, to prevent withdrawal symptoms including withdrawal delirium. At all times use clinical judgment; pharmacy can assist with medication/dose adjustments as appropriate.
What Else Can I Do About It?
Consider the following actions, as clinically appropriate:
1. Review RISK FACTORS
MODIFIABLE risk factors for delirium include:
- ICU level of care
- Mechanical Ventilation >24 hrs
- New surgical procedure
- Use of high risk medications
NON-MODIFIABLE risk factors for delirium include:
- Age > 70
- Baseline dementia or cognitive impairment
- Baseline functional or mobility impairment
- History of delirium
- History of drug or alcohol misuse
- Two or more chronic health conditions
- Vision and/or hearing impairments
2. Identify and Treat UNDERLYING CAUSES (DELIRIUM)
- Drugs (adverse effects, high risk medications*)
- Electrolyte disturbances (Na+, Ca++, others)
- Lack of drugs (i.e., drug withdrawal: consider baseline alcohol, opioid, tobacco, and anxiolytic use)
- Infection/sepsis and/or new organ failure
- Reduced sensory input (poor hearing, poor vision)
- Intracranial (CNS infection, stroke, ICH, tumor, seizure)
- Urinary (retention, incontinence)
- Undernutrition, Underhydration, Undermobilized
- Myocardial/pulmonary (hypoxia, hypercarbia, acute MI, decompensated CHF, COPD)
- Others: constipation, undertreated pain, boredom/poor social support, sleep deprivation
3. Review and Manage PRECIPITATING TRIGGERS
- Limited mobility: Set challenging daily mobility goals; consult PT/OT; remove tethers like physical restraints, telemetry, foley catheters, IVs with continuous fluids unless medically necessary
- Malnutrition: Provide feeding assistance as needed, consult dietitian, order nutritional supplements
- Urinary retention: Check bladder scans
- Urinary incontinence: Consider scheduled toileting
- Constipation: Provide bowel regimen, early and frequent mobilization
- Overstimulation: Remove unnecessary devices; if devices can’t be removed, ensure they are untethered, secure, and camouflaged
- Sleep deprivation: Provide ear plugs/eye masks; limit daytime sleeping; keep room lights ON during daytime and turn OFF at night
- Communication barriers: Ensure hearing aids and eyeglasses used if applicable; provide communication aids and/or involve SLP
- Poor social/cognitive support: Encourage/support family interaction; provide cognitive stimulating activities
- Active/undertreated pain: Consider scheduled acetaminophen [no more than 3-4 g/24h]; provide non-pharmacologic measures to reduce pain, including mobilization/repositioning
- Use of high risk medications: Discontinue/reduce high risk medications as clinically appropriate
4. INVOLVE THE PATIENT’S FAMILY MEMBER/NEXT OF KIN in decisions and transitions of care.
5. CONSIDER CONSULTATION with geriatrics (if 65+), behavioral health and/or neurology.
What About Antipsychotics?
In general, there is no compelling evidence supporting the efficacy of antipsychotics for the treatment of acute inpatient delirium. However, antipsychotics may be considered for moderate or severe agitation in delirium, or if delirium interferes with care despite treating the underlying cause(s).
Additional Resources
Learn more at:
Coming Soon
- Delirium toolkit items (useful for distraction, avoidance of restraints) will soon be available for nursing staff to order through central supply.
- The Cerner “Delirium Powerplan” is being built, but it is not yet live.